Patellar Dislocation
Let’s understand Patellar Dislocation
Patellar Dislocation
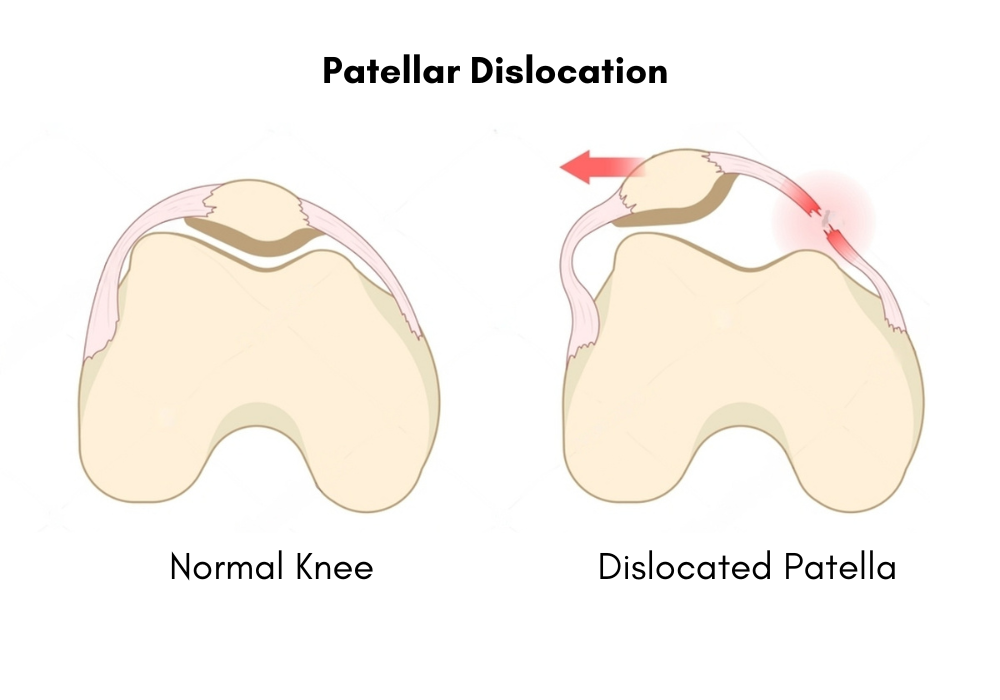
Patellar dislocation occurs when the patella (kneecap) is displaced from its normal position within the trochlear groove of the femur (thigh bone). This condition is often the result of trauma or sudden twisting movements, especially during sports or accidents. Anatomical predispositions, such as a shallow trochlear groove, high-riding patella (patella alta), or ligamentous laxity, can increase the likelihood of dislocation. Muscle imbalances, particularly in the quadriceps, also contribute to instability and a higher risk of patellar dislocation.

Patellar Dislocation
Patellar dislocation occurs when the patella (kneecap) is displaced from its normal position within the trochlear groove of the femur (thigh bone).
What are the causes ?
When the kneecap is moved out of its natural place inside the trochlear groove at the end of the thigh bone, it results in patellar dislocation. Numerous factors can contribute to this displacement, such as trauma from falls or direct impacts on the knee, anatomical abnormalities such as a shallow trochlear groove or misalignment of leg bones, muscle imbalances, especially in the quadriceps and hamstrings, joint laxity, history of knee injuries weakening supporting structures, participation in sports or activities involving repetitive twisting or abrupt changes in direction, genetics, and specific medical conditions like hypermobility syndromes. Patellar dislocation risk can also be influenced by age, gender (females are more prone to it), and underlying genetic predispositions.


What are the symptoms ?
The severity of the dislocation and any accompanying injuries can affect the symptoms of patellar dislocation, but common ones include sudden, excruciating pain around the kneecap, knee joint swelling and tenderness, difficulty bending or straightening the knee, and, in extreme cases, a visible displacement of the kneecap. A popping or snapping feeling may also be felt by some people at the moment of the dislocation. There may be persistent pain following the original injury, particularly while moving or bearing weight. Chronic pain, instability, and a feeling that the knee is “giving way” when doing physical tasks can result from recurrent dislocations.If you encounter any of these symptoms, it’s critical to get medical aid right away because timely care can help stop more harm from occurring and enhance results.
Treatments
Surgical Intervention:
Medial Patellofemoral Ligament (MPFL) reconstruction
Medial Patellofemoral Ligament (MPFL) reconstruction is a surgical procedure designed to enhance knee stability and reduce the risk of recurrent patellar dislocations. The MPFL is a key ligament that helps maintain the patella’s position within the trochlear groove. When this ligament is torn or damaged, typically due to dislocation, the patella becomes prone to subsequent dislocations. MPFL reconstruction involves creating a new ligament using a graft, often taken from the patient’s own hamstring tendon. This graft is then anchored to the femur and patella, restoring the stabilizing function of the MPFL. The procedure is particularly effective for patients with recurrent patellar instability and significantly improves knee stability, allowing for a return to normal activities and sports.
Tibial tubercle osteotomy
Tibial tubercle osteotomy is another surgical technique used to correct patellar malalignment and improve patellar tracking. This procedure is indicated in cases of severe malalignment where the patella does not move smoothly within the trochlear groove, often causing pain and recurrent dislocations. The tibial tubercle, the bony prominence on the tibia where the patellar tendon attaches, is surgically repositioned to alter the alignment and tracking of the patella. By changing the position of the tibial tubercle, the surgeon can adjust the forces acting on the patella, ensuring it tracks properly within the groove. This procedure helps reduce pain and improve knee function, particularly in patients with chronic misalignment issues.
Cartilage repair techniques
Cartilage repair techniques are crucial in addressing damage to the articular cartilage of the knee joint, which often accompanies patellar dislocations or other knee injuries. Healthy cartilage is essential for smooth joint movement and cushioning. When cartilage is damaged, it can lead to pain, swelling, and decreased mobility. Several techniques can be used to repair cartilage damage. Microfracture involves creating small holes in the underlying bone to stimulate the growth of new cartilage. Cartilage transplantation, or osteochondral autograft transfer, involves transferring healthy cartilage from a non-weight-bearing area of the joint to the damaged area. Autologous chondrocyte implantation (ACI) involves harvesting cartilage cells from the patient, culturing them in a lab to increase their number, and then implanting them back into the damaged area. These cartilage repair techniques aim to restore the smooth surface of the joint, alleviate pain, and improve knee function, allowing patients to return to their normal activities.
Exploring Post Surgical Management
The goals of post-surgical care for patellar dislocation operations are to promote healing, regain function, and stop further dislocations.
Protection and Immobilization:
To safeguard the surgical site and promote tissue healing, the knee may be immobilized following surgery with a brace or splint. At first, weight-bearing may be limited, and crutches or a walker may be utilized to help with mobility.
Pain Management:
To control pain and suffering following surgery, doctors may prescribe prescription or over-the-counter painkillers. Pain and swelling can also be lessened with ice therapy.
Physical Therapy:
An essential part of the recovery process following surgery is physical therapy. To start, passive range-of-motion exercises can be done to encourage circulation and prevent stiffness. Active range of motion activities, hamstring and quadriceps strengthening exercises, and proprioceptive exercises to enhance balance and coordination may be added as the healing process advances.
Bracing and Support:
A knee brace or patellar stabilizing brace may be worn during activities to give extra support and stability, depending on the type of surgery done and the surgeon’s wishes.
Monitoring & Follow-up:
To keep an eye on developments, resolve any issues or difficulties, and modify the rehabilitation plan as necessary, follow-up sessions with the surgeon and physical therapist are crucial.
Education and Lifestyle Changes:
To lower the likelihood of recurrent dislocations, patients will receive education on appropriate body mechanics, strategies for modifying their activities, and lifestyle changes. To lessen strain on the knees, this may entail staying away from activities that put an excessive amount of stress on the knee joint and keeping a healthy weight.
Psychological Support:
Knee surgery recovery can be emotionally and physically taxing. Patients can maintain their motivation and involvement in their rehabilitation program by receiving psychological support and encouragement during the healing process.



Schedule An Appointment
Elevate your performance with Apex Sports Clinic! Schedule an appointment today for personalized, expert care in optimizing your athletic potential.


APEX SPORTS CLINIC
Search Here
Book An Appointment
Quick Links
Contact us
- Email Address
- admin@apexsportsclinic.sg
- Address
- #18-12, Royal Square Medical Center,101 Irrawaddy Road, Novena, Singapore 329565
- Phone
- +6587745468
- Address
- #03-03/04, i12 Katong, 112 East Coast Road, Singapore 428802
- Phone
- +6583219004
APEX SPORTS CLINIC
Search Here
Book An Appointment
Quick Links
Contact us
- Address
- #18-12, Royal Square Medical Center,101 Irrawaddy Road, Novena, Singapore 329565
- +6587745468
- Address
- #03-03/04, i12 Katong, 112 East Coast Road, Singapore 428802
- +6583219004
- Email Address
- admin@apexsportsclinic.sg

APEX SPORTS CLINIC
Quick Links
Search Here
Book An Appointment
Contact Us
- Email Address
- admin@apexsportsclinic.sg
- Address
- #18-12, Royal Square Medical Center,101 Irrawaddy Road, Novena, Singapore 329565
- Phone
- +6587745468
- Address
- #03-03/04, i12 Katong, 112 East Coast Road, Singapore 428802
- Phone
- +6583219004